When we think of animation, we picture illustrations and digital storyboards coming to life. When a person shares exciting news in a happy state we say, “don’t they look animated?” Now, the phrase ‘re-animate’ has an entirely different meaning in the world of medicine — to bring a person back to life.
Medical enthusiast, Dr. Natalie Kruit is exploring a newfound technology that is set to take Sydney (and Australia) by storm. After completing a degree in Psychology and Nursing, the mother of two was determined to take it one step further. When her heart led her to complete a medical degree at the University of Sydney, she soon realised that her role was to shift perspectives as a formidable medic.
After spending ten years training to be a specialist cardiac anaesthetist at Westmead Hospital, Natalie qualified as an Anaesthetist, specialising in resuscitation and reanimation. Natalie explained, “It still amazes me how the heart can restart after it stops – the heart is at the core of everything. Without it, things just don’t work”.
This is very true, on so many levels.
As a self-confessed adrenalin chaser with a desire to help those literally on a cliff’s edge, Natalie rotates as an onboard doctor with NSW Rescue Helicopters. “Being able to save people who would otherwise not make it, is why I do what I do”, says Natalie. “Resuscitation and reanimation is at the pointiest edge of medicine. As a doctor, this is ultimately what we strive for. To save lives”.
During a twelve-month traineeship in the UK, she received specialist training in a new and ground-breaking piece of technology, Cardiohelp. Natalie describes Cariohelp as the tech-box that increases the chances of survival tenfold.
This ‘box’ performs Extracorporeal Membrane Oxygenation (ECMO). The ECMO procedure — otherwise known as the E-CPR technique — is a digital device that can drain all the blood from a patient, pump it into a machine, oxygenate the blood, remove the waste, and pump it back into the patient. All whilst their heart and lungs are essentially failing.
In the early 1970’s, ECMO research began with adults but quickly turned to newborns with breathing problems. Dr Robert Bartlett, the creator of ECMO successfully treated the first newborn in 1975 in Irvine, California. Now, this technology can be seen around the world.
With a rise in respiratory patients due to the Coronavirus pandemic this technology is needed more than ever. A specialist hospital in France has seen an increase from 20 patients per month to a further (and frightening) two hundred admissions needing this life-saving treatment. Seeing a surge of patients admitted for this treatment, the specialist French team who coined the first hospital to house ‘The Reanimation Department’, continue to perform this ground-breaking procedure.
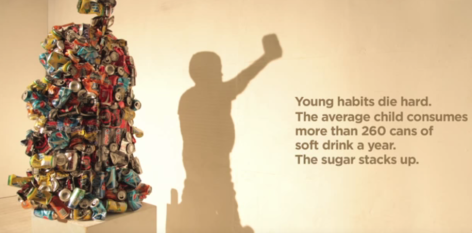
When a heart stops, there is a 5-8% chance of survival if cardiopulmonary resuscitation (CPR) does not work in the first twenty-minutes. For the last seven years, E-CPR has been active in hospitals, increasing the survival rate by 33%. But, for every minute in cardiac arrest after thirty-minutes, there is a 2.5% mortality rate increase.
The recent landmark ‘ARREST’ trial has demonstrated a 100% survival rate if the patient is on ECMO in less than 30 mins. This is game changing!
Natalie — the only doctor in Australia equipped to perform pre-and in-hospital reanimation using this device — questioned, ‘‘how can we use this technology to reanimate life on the streets of Sydney?”. She now wants to take this procedure into the city’s busy metropolis — especially as this can be hard for emergency response vehicles to navigate. “If we can do this on any walkway, we can up the chances of survival by a staggering 50%,” she predicts.
“When the next ‘000’ call comes in, I want to see this technology onboard with a doctor equipped to use it”.
As a humanitarian in medicine, Natalie’s passion is clear.
“Walking into a room offering hope to patients and their families when all hope has been lost is everything,” she says. “When the local hospital has exhausted all other treatment, this technology can alter that.”
Natalie says critical care is simply her passion — and it’s never more important than in the wake of a pandemic.
“One patient of mine had coronavirus,” says Natalie “She was supported with this technology for six weeks. It never came off. The machine essentially was a digital lung and until her body recovered, we continued this treatment. Now she practices Zumba five times a week”.
To save Sydneysiders at the scene of a Cardiac Arrest, this technology doesn’t come without its challenges. Natalie is at the forefront of a campaign to raise both awareness and funds to support this medical trial with each device costing $250k. “Every researcher and health care professional will advocate for a treatment close to their heart, but this device is for the heart,” she says. “This will save so many more lives! My job now is to convince my peers why”.
As a medical entrepreneur, Natalie is inspired to integrate cutting-edge technology at the curbs and on the cliff topsof Australia. As the only doctor in Australia trained to perform this procedure outside of a hospital setting, Natalie is certainly determined – and reanimation just became a lot more life-like.